What happens if I don’t participate in MIPS?
If you exceed the low volume threshold and do not participate, a - 9% adjustment will be applied to your Medicare Fee-for-Service(FFS) reimbursement in 2022. This is easy to avoid with minimum effort on your part. You just need some guidance to get you there.
Why should I opt in to participate?
Every practice is already doing the work, so it makes sense that you would capitalize on the extra revenue. Depending on how well you do, you could even receive part of the $500 million that is still available for disbursement.
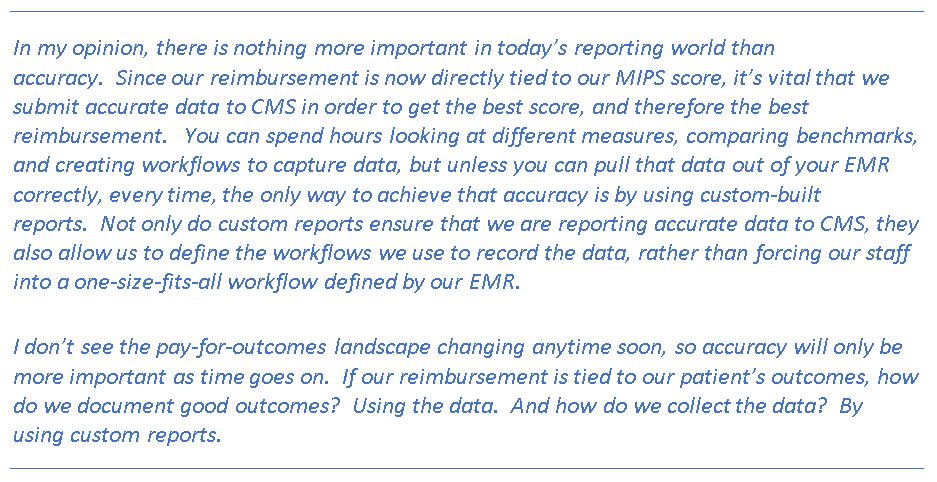
Accuracy is an imperative piece of quality reporting. If your current Quality or Promoting Interoperability reports are not reflecting your high level of performance, you should contact eHealth about custom reporting. We combine the specifications with your individual practice workflow to reflect your high level of performance.
How do I know I am eligible for MIPS?
Check the Quality Payment Program Eligibility Page. This page is integrated with PECOS. When you enter your NPI, youI will get a report of all of the Tax ID numbers (TIN) that the NPI is actively associated with and whether or not the eligible clinician is able to participate as an individual clinician or group, or is perhaps part of an Advanced Payment Model (APM).
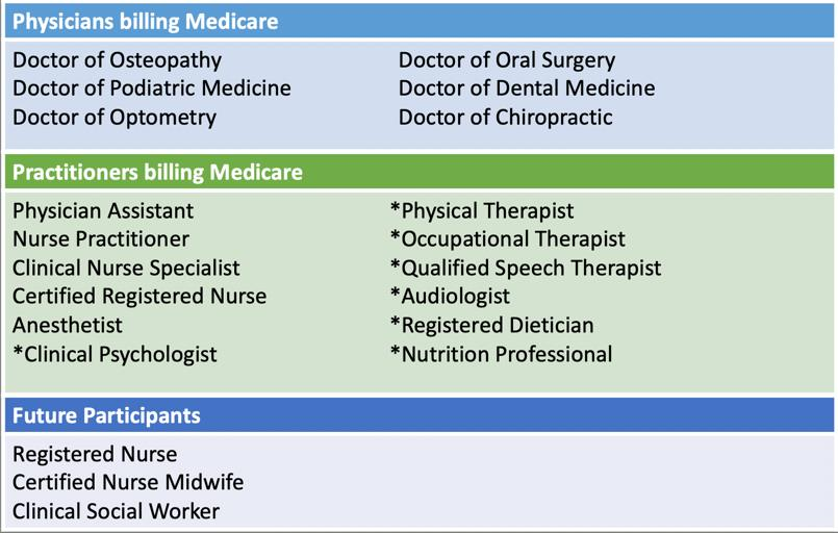
I like to think of eligibility as a two-step process. First, is the clinician in the list of eligible clinicians?. Second, did that clinician meet the low volume threshold as an individual or group?.
What is the difference between participating as an individual versus a group?
First, a group is defined as two or more eligible clinicians under the same TIN that have reassigned their billing rights over to the TIN. There is a virtual group definition as well, but it is hardly worth mentioning since so few practices are participating through this method.
There are several reasons I can think of for participating as a group versus an individual, but the most important is that it opens the door for all eligible clinicians in the group to receive the positive payment adjustment, even if they do not meet the low volume threshold individually. I am all about an opportunity to increase revenue for the practice!
Choosing to participate as a group also means that data from all eligible clinicians, regardless of whether they meet the low volume requirements or not, must be included in the aggregated scores for all the MIPS categories the group submits.
MIPS Scoring Thresholds
Threshold to avoid a negative payment adjustment = 45
Threshold for Exceptional Performer Status = 85